Introduction
Every audiologist knows this story. A patient walks in desperate for help with the constant ringing in their ears. You create a thoughtful treatment plan and send them off with hope. Three weeks later, they’re a no-show for their follow-up. Another patient lost before seeing real results.
The numbers don’t lie, up to 40% of tinnitus patients abandon treatment prematurely. This revolving door not only leaves people suffering unnecessarily but also impacts your practice’s bottom line and professional satisfaction.
In this blog, we’ll show you proven strategies that transform patient retention while delivering better outcomes for those suffering from tinnitus. These approaches work for any practice, regardless of size.
Why Patients Drop Out of Tinnitus Treatment
Tinnitus affects about 50 million Americans, yet traditional management approaches often fail to keep patients engaged long-term for several reasons:
First, tinnitus is invisible. Unlike hearing loss that shows clearly on an audiogram, tinnitus exists only in the patient’s experience. Without measurable benchmarks, patients can’t recognize their own progress.
Second, improvement happens slowly. Without clear milestones, patients get discouraged and quit before experiencing meaningful relief.
Third, tinnitus is highly individualized. One-size-fits-all approaches rarely work consistently across your patient population.
These factors create the perfect storm for patient dropouts. But with smart data use and clear frameworks, you can transform your retention rates dramatically.

A Better Approach to Tinnitus Management
The most successful tinnitus programs position patients as active participants in their recovery journey. Here are 8 proven tinnitus therapy strategies to improve patient retention and results:
1. Always Put Your Patient First
Tinnitus patients typically arrive feeling helpless. Your job is to reframe their situation, helping them see themselves as capable of overcoming their challenge with your guidance. Data collection becomes their tool for tracking progress.
2. Be Their Support System
Your role combines both empathy and expertise:
Show understanding: “I see your sleep scores have dropped this week. That must be frustrating after the progress you were making.”
Share expertise: “When we’ve worked with patients showing similar patterns, 83% improved significantly when we adjusted their therapy this way.”
3. Create a Clear Roadmap
Tinnitus patients need a crystal-clear plan:
⦁ Measure baselines across multiple dimensions (loudness, annoyance, sleep impact)
⦁ Set achievable milestones based on typical progress patterns
⦁ Schedule regular check-ins tied to specific measurements
⦁ Show progress visually so improvement becomes obvious
⦁ Make treatment adjustments based on actual results
This structured approach gives patients confidence in your recommendations and their journey.
4. Simple Data Collection Anyone Can Implement
You don’t need complex systems to become data-driven. Here are practical approaches any practice can use:
Start With Basic Assessments
Begin with proven measurement tools:
⦁ Tinnitus Handicap Inventory (THI): Measures overall life impact through 25 questions covering functional, emotional, and catastrophic reactions to tinnitus.
⦁ Tinnitus Functional Index (TFI): Breaks down impacts by category across 25 items in eight subscales: intrusiveness, sense of control, cognitive interference, sleep disturbance, auditory difficulties, relaxation issues, quality of life, and emotional distress.
⦁ Tinnitus Reaction Questionnaire (TRQ): Focuses specifically on psychological distress with 26 items measuring anxiety, depression, and anger responses to tinnitus.
⦁ Visual Analog Scales (VAS): Simple 1-10 ratings for key symptoms like loudness, annoyance, and impact on daily life.
⦁ Pittsburgh Sleep Quality Index (PSQI): Tracks sleep disturbances through 19 self-rated questions that create seven component scores.
These assessments create your baseline and give you and your patients a shared language for discussing progress.
Use Regular Quick-Checks
Between major assessments, collect brief data points:
⦁ Weekly mini-surveys (under 2 minutes to complete)
⦁ Daily symptom tracking for key metrics
⦁ Therapy usage logs showing how consistently patients follow recommendations
These quick check-ins provide valuable clinical information while keeping patients engaged with their treatment.
Make Data Collection Easy
If it’s complicated, patients won’t do it:
⦁ Use simple rating scales (1-5 or 1-10)
⦁ Keep it brief (5 questions max for regular check-ins)
⦁ Show completion time (“Takes less than 90 seconds”)
⦁ Give immediate feedback (“Your sleep score improved 20% this week!”) The best system is the one patients will actually use.
5. Turn Data into Patient Engagement
Collecting data is just the first step. Here’s how to transform those numbers into better patient retention:
Create Visual Progress Reports
People process visual information better than raw numbers:
⦁ Generate simple line graphs showing improvement trends over time. For example, plot THI scores across appointments to show the downward trend that might not be obvious from just looking at numbers.
⦁ Use color-coding to highlight progress (green) and areas needing attention (yellow). This creates instant visual understanding, patients immediately grasp “green means good” without requiring detailed explanation.
⦁ Show percentage improvements compared to baseline. Instead of saying “Your THI score went from 62 to 48,” say “You’ve experienced a 23% reduction in tinnitus impact on your daily life.”
⦁ Note when treatment changes were made to show cause-and-effect relationships. This helps patients connect your interventions with their improvements, reinforcing the value of your recommendations.
When patients can see their progress, their motivation to continue treatment soars.
Personalize Based on Data Patterns
Use collected data to customize treatment:
⦁ Identify which therapy approaches work best for each individual by correlating usage patterns with outcome improvements. If a patient shows the most significant drops in distress scores after using specific relaxation techniques, prioritize and expand those methods.
⦁ Recognize patterns in symptom flare-ups and address triggers proactively. For example, if data shows tinnitus distress increases consistently during high-stress work periods, implement preventative strategies before these known challenging times.
⦁ Adjust appointment frequency based on actual needs rather than arbitrary schedules. Some patients may need weekly support during difficult phases but can maintain progress with monthly check-ins during stable periods.
⦁ Recommend specific techniques based on individual response patterns. The data might reveal that certain patients respond exceptionally well to mindfulness exercises while others benefit more from environmental sound enrichment.
When patients see their feedback directly shaping their treatment, they develop deeper trust.
Use Practice-Wide Statistics
While maintaining privacy, use your aggregated data to build confidence:
“Based on data from over 200 patients with similar profiles, 72% experience significant reduction in tinnitus distress within 12 weeks when following this protocol consistently.”
This leverages social proof while showing your recommendations are evidence-based.

6. Create a Bulletproof Follow-Up System
The best data means nothing without consistent follow-up. Here’s how to prevent patients from falling through the cracks:
Design a Smart Follow-Up Schedule
Create a standard progression that adapts to patient data:
⦁ First month: Weekly brief check-ins with mid-point assessment
⦁ Months 2-3: Bi-weekly monitoring with monthly assessments
⦁ Months 4-6: Monthly check-ins with quarterly assessments
This structure reassures patients while maximizing staff efficiency.
7. Set Up Warning Flags
Establish automatic alerts for potential dropout signals:
⦁ Two consecutive missed data submissions: This often represents the first sign of disengagement. When patients stop tracking, they’re mentally checking out of the treatment process. A quick outreach at this stage can prevent complete abandonment.
⦁ 20% increase in distress scores: Sudden jumps in symptom severity frequently lead to frustration if not addressed quickly. These spikes may indicate new triggers, treatment tolerance issues, or life changes affecting the patient’s condition.
⦁ Sudden changes in sleep quality: Sleep disruption represents one of the most distressing aspects of tinnitus for many patients. Deteriorating sleep metrics often precede treatment dropout if not promptly addressed.
⦁ Declining therapy compliance: When patients report decreasing adherence to recommended strategies, they’re signaling doubt about effectiveness. This warning sign provides an opportunity to address concerns, adjust approaches, or provide renewed motivation.
When these triggers occur, reach out personally: “I noticed your scores increased last week. Let’s schedule a quick call to make some adjustments to your plan.” This proactive approach shows patients you’re monitoring their progress between appointments.
8. Train Your Entire Team
Your whole staff should understand and support your data approach:
⦁ Front desk checks assessment completion at check-in
⦁ Clinicians reference specific data points during consultations
⦁ All team members can explain why tracking matters
When everyone communicates consistently, patients receive constant reinforcement of the process’s value.
Your Action Plan: Start Tomorrow
⦁ Select 2-3 core assessments that address your patients’ most common concerns
⦁ Create a simple baseline protocol for consistent initial measurement
⦁ Develop basic visualization tools to demonstrate progress visually
⦁ Establish a follow-up schedule with clear responsibility assignments
⦁ Train your team on both the process and the reasoning behind it
Remember, perfect is the enemy of progress. Start simple, measure consistently, and refine your approach as you learn.
Conclusion:
The practices that thrive in tinnitus management aren’t necessarily those with the most advanced equipment or techniques, they’re the ones that help patients see and believe in their own progress. With the right data approach, your practice can become a retention powerhouse while delivering the outcomes your patients desperately need.
Ready for a Partner Who Helps You Keep Patients Engaged?
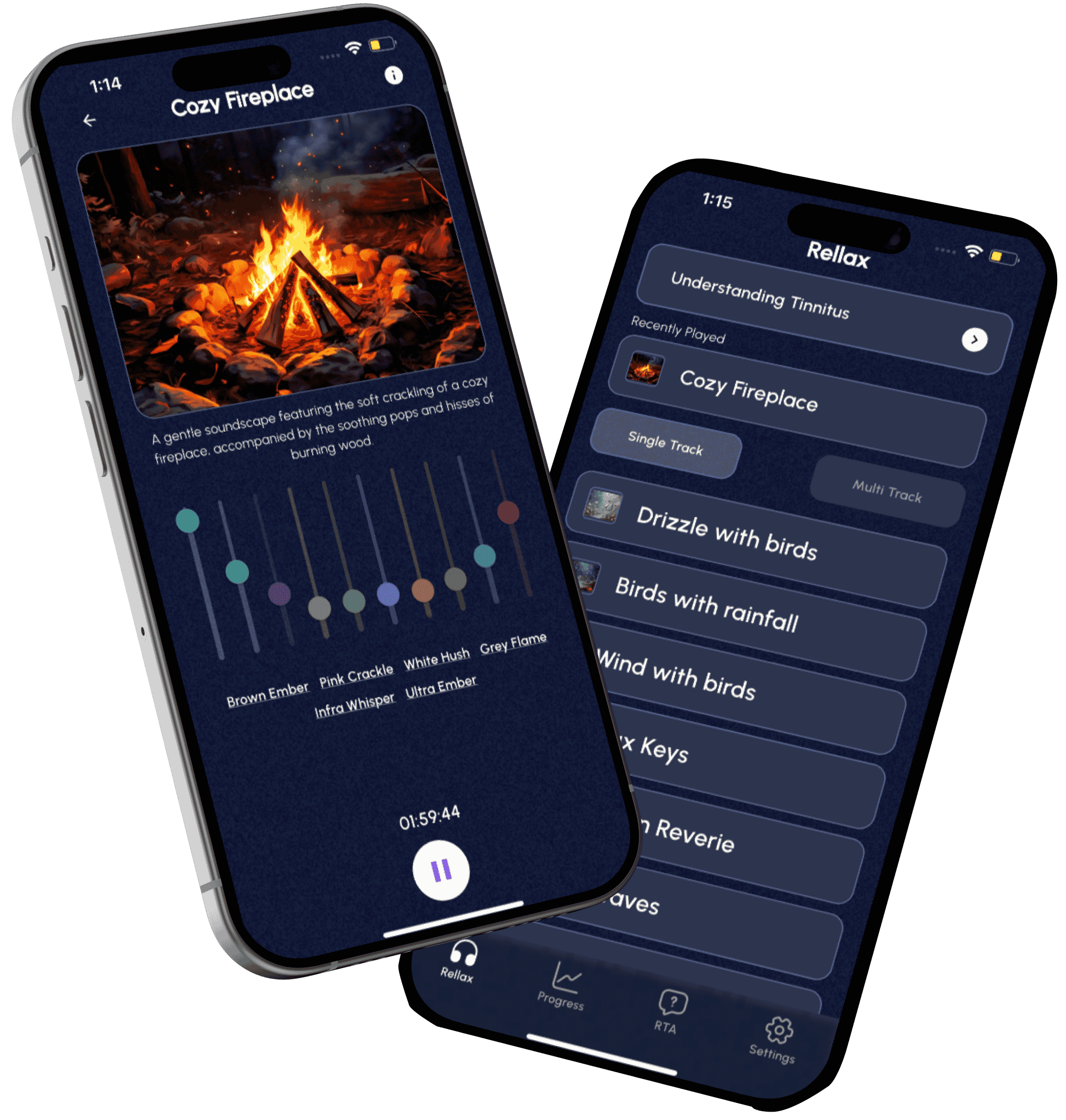
If you want more support in making data-driven decisions, keeping patients motivated, and personalizing tinnitus therapy at scale, Rellax is here to help.
We’re not just an app, we’re your partner in creating better outcomes, reducing drop-offs, and helping more patients find real relief.
Schedule a FREE walkthrough to see how Rellax can integrate with your clinic and support your mission to heal. Email us at ryan@rellax.co or visit https://rellax.co/providers/.
Frequently Asked Questions (FAQs)
Progress varies, but with personalized, data-driven therapy like Rellax, patients often start noticing changes in sleep, mood, or tinnitus perception within 2–4 weeks. Visual progress tracking helps them stay motivated.
Yes. When patients see measurable progress and know their therapy is tailored to their experience, they feel more in control and are more likely to complete the program. This is supported by TRQ and other behavioral data.
Not at all. Rellax integrates smoothly into your existing practice. You can start by offering it to a few patients and expand as you see results. It’s a flexible and scalable solution built for busy clinics.
Have any question?
Do not hesitate to contact us. We’re a team of experts ready to talk to you.
ryan@rellax.co
5 Data-Backed Strategies to Improve Patient Outcomes for Tinnitus Management
Introduction
Tinnitus is one of the most cumbersome challenges in audiology. No two patients present the same symptoms, and treatment outcomes can vary dramatically, even when using the same approach. The unpredictable nature of tinnitus, combined with the emotional toll it takes on patients, often leaves audiologists searching for better, more consistent strategies.
As expectations for personalized care grow, audiologists are now turning to tools and techniques grounded in data, ongoing tracking, and tailored therapy. The days of one-size-fits-all are over.
In this blog, we’ll walk through five data-backed strategies that can help you improve tinnitus therapy, increase patient engagement, and ultimately deliver better tinnitus treatment outcomes, all while streamlining your clinical workflow.
Let’s dive in.

1. Use Standardized Tinnitus Assessment Tools
Before diving into treatment, it’s crucial to understand the full scope of your patient’s symptoms. Tinnitus presents differently for everyone. Some patients hear a faint hum, while others experience a loud, distressing ring.
Standardized tinnitus assessment tools help you gather clear, measurable information about how tinnitus impacts your patient’s daily life. This makes it easier to create a treatment plan tailored to their unique experience.
What the Data Says:
A 2024 study published in The Journal of Audiology found that clinics using standardized assessment tools like the Tinnitus Handicap Inventory (THI) were able to adjust treatments more effectively, resulting in a 28% improvement in patient-reported outcomes within the first three months of therapy. By leveraging these tools to monitor symptom changes, audiologists were able to identify effective interventions more quickly and minimize trial-and-error in treatment approaches.
Common Tools Used in Tinnitus Assessment:
Tinnitus Handicap Inventory (THI):
A 25-question survey measuring emotional, functional, and catastrophic responses to tinnitus.
Tinnitus Functional Index (TFI):
Assesses the impact of tinnitus on various aspects, including sleep, concentration, and emotional well-being.
Visual Analog Scales (VAS):
Simple 0–10 scales measuring the perceived loudness, annoyance, or distress caused by tinnitus.
Tinnitus Reaction Questionnaire (TRQ):
A 26-item questionnaire that evaluates the emotional distress associated with tinnitus, including anxiety, depression, and irritability. It helps audiologists understand how tinnitus is affecting a patient’s mental health and quality of life.
Why These Tools Matter:
By using standardized assessment tools, you can objectively measure the impact of tinnitus, track symptom progression, and adjust interventions accordingly. This structured approach ensures that treatment plans are personalized and responsive to your patient’s specific experience.
2. Match the Sound to the Symptom: How Personalized Therapy Helps
Every tinnitus patient is unique. The intensity and frequency of the ringing sound they hear can vary from person to person, making it essential to provide personalized sound therapy that addresses each patient’s specific symptoms.
What the Data Says:
A meta-analysis conducted by JAMA Otolaryngology in 2020 found that personalized sound therapy was significantly more effective than generic sound therapy in reducing tinnitus intensity. Patients who received sound therapy tailored to their specific frequency and pitch of tinnitus experienced a 40% reduction in perceived tinnitus severity.
How to Implement Personalized Sound Therapy:
Symptom Matching Algorithms:
Tools like Rellax use symptom profiling algorithms to create personalized sound therapy based on the patient’s tinnitus characteristics. This can include matching sound frequencies, volume, and tone to the patient’s specific tinnitus pattern, enhancing the effectiveness of the therapy.
Find the Blend Point:
One important technique is identifying the blend point, the frequency and volume where the therapeutic sound merges with the patient’s tinnitus sound. At this point, the brain begins to filter out the tinnitus more easily, reducing its perceived intensity. Using the blend point helps patients achieve quicker relief and greater comfort during therapy.
Adaptive Sound Libraries:
Sound therapy can include a wide range of audio options, such as nature sounds, white noise, or calming music. However, many modern tinnitus management tools now follow the principles of Tinnitus Retraining Therapy (TRT), which emphasizes the use of broadband noise. This type of sound is designed to blend with the tinnitus signal and help the brain gradually tune it out. Platforms like Rellax are built around this concept, offering customizable broadband sound options that support consistent and comfortable therapy. By adapting the sound stimuli to each patient’s tinnitus profile and comfort level, therapy becomes more effective and easier to stick with.
Why It Works:
Personalized sound therapy helps patients focus on specific frequencies that are tolerable to the patient, reducing the perceived intensity of the sound. When patients use tailored therapies, they’re more likely to adhere to treatment and experience better long-term results.

3. Address the Mind: Combining CBT with Sound Therapy
It’s not just about treating the ears; it’s also about treating the mind. Many patients with tinnitus experience anxiety, depression, and distress, which can worsen their symptoms. Combining sound therapy with cognitive behavioral therapy (CBT) is a highly effective way to address both the physical and psychological aspects of tinnitus.
What the Data Says:
A study published in The Lancet showed that patients who underwent both CBT and sound therapy experienced a 50% reduction in tinnitus-related distress within six months. CBT helps patients reframe negative thoughts, reducing the emotional burden of the condition.
How to Implement CBT:
Partner with Mental Health Professionals:
Collaborating with licensed mental health professionals can help you offer CBT in conjunction with sound therapy.
Offer CBT Modules through Tinnitus Apps:
Many tinnitus management platforms now offer guided CBT sessions as part of their treatment plans, which patients can access remotely.
Why It Works:
CBT helps patients change the way they perceive their tinnitus, making it less distressing. When combined with sound therapy, CBT provides a comprehensive approach that treats both the physical and emotional aspects of tinnitus.
4. Keep Patients on Track: Why Consistency Makes All the Difference
Consistency is key when it comes to managing tinnitus. Many tinnitus therapies, including sound therapy and cognitive behavioral therapy (CBT), require patients to stay engaged in their treatment. Ensuring therapy adherence can significantly improve treatment outcomes.
What the Data Says:
A study published in The Journal of the American Academy of Audiology found that clinics using digital tracking tools saw a 25% increase in therapy adherence and a 35% decrease in patient dropout rates. When patients feel supported and engaged, they’re more likely to stick to their treatment plan.
How to Monitor Patient Engagement:
Patient Management Dashboards:
Tools like Rellax’s patient dashboard allow audiologists to monitor patient progress in real time. These platforms can track patient engagement, session completion, and symptom changes, providing audiologists with valuable insights into how well patients are adhering to their treatment plans.
Automated Reminders:
Apps or email reminders encourage patients to stay on track, reinforcing the importance of consistent treatment.
Why It Works:
Better engagement leads to better outcomes. When patients are actively involved in their tinnitus management, they’re more likely to experience positive results. Digital tools help make engagement seamless, improving the overall treatment process.
5. Use Outcome Data to Continuously Optimize Therapy
The best way to improve tinnitus therapy is by making data-driven decisions. Continuously tracking patient progress and using outcome data to refine treatment plans helps audiologists deliver more effective and personalized care.
What the Data Says:
A 2024 study published in the Journal of Otolaryngology used high-frequency audiometry data with machine learning models and achieved over 94% accuracy in diagnosing tinnitus. This proves that data isn’t just useful, it’s essential for improving diagnosis and ongoing care.
Moreover, industry reports highlight that audiology practices using digital dashboards and trend analysis tools are reducing dropout rates and increasing therapy adherence by 30–40%.
How to Use Outcome Data:
Track Progress with Patient Feedback:
Collect patient feedback regularly, either digitally or in person, to assess progress and identify areas for improvement.
Use Trend Analysis to Adapt Therapy:
Analyzing trends in patient data helps identify patterns. If a patient’s tinnitus intensity worsens, therapy can be modified promptly.
Why It Works:
Real-time data allows audiologists to adapt treatment quickly. By continuously optimizing therapy, audiologists can ensure that patients receive the best possible care throughout their treatment journey.

Conclusion
Improving patient outcomes for tinnitus management requires a combination of personalization, consistent tracking, and evidence-based interventions. By integrating standardized tinnitus assessment tools, personalized sound therapy, and mental health support like CBT, audiologists can offer more comprehensive and effective treatment. Additionally, using outcome data to continuously refine therapy plans ensures that patients receive the best possible care.
If you’re looking for a tool that can help streamline tinnitus management, improve patient engagement, and enhance treatment outcomes, Rellax offers a comprehensive, evidence-based solution. By incorporating personalized sound therapy and real-time patient monitoring, Rellax empowers audiologists to provide better care and achieve better results for their tinnitus patients.
Join the Rellax Partner Program Today!
Frequently Asked Questions (FAQs)
1. What is the most effective treatment for tinnitus in 2025?
The most effective treatment depends on the individual, but combining sound therapy with behavioral interventions like CBT, while continuously tracking patient progress, leads to better outcomes.
2. How can I improve my patients’ tinnitus therapy outcomes?
Use standardized assessment tools, track therapy adherence, apply outcome data regularly, and integrate CBT techniques alongside sound therapy for comprehensive support.
3. Is there a data-driven way to manage tinnitus more effectively?
Absolutely. Audiologists using digital platforms and analytics tools have reported up to a 45% improvement in tinnitus treatment outcomes by adapting therapy based on real-time data.