Introduction
Tinnitus, the perception of sound without an external source affects approximately 15% of the population, with a subset experiencing significant distress necessitating clinical care. As audiologists, it is crucial that our clinical decisions reflect not just the science but also the lived realities of our patients.
This blog highlights recent patient insights and actionable strategies clinics can implement immediately to better meet patient expectations and improve outcomes.
How Patients Describe Their Experience
Patients’ descriptions go beyond “ringing in the ears.” People commonly report ringing, buzzing, whooshing, hissing or pulsatile sounds; more importantly they describe the emotional and functional toll: sleep disruption, concentration problems, anxiety, social withdrawal and reduced work productivity. Qualitative studies show tinnitus can feel like an “invisible prison” for some sufferers.

When working with tinnitus patients:
- Ask patients to describe how tinnitus impacts their day (sleep, mood, work, relationships) rather than only characterizing sound.
- Use validated PROMs (e.g., Tinnitus Handicap Inventory) alongside open, empathetic questioning.
What Patients Want
1) Recognition and Validation
A frequent patient complaint is feeling dismissed or told “learn to live with it.” Patients don’t just want treatment, they want their experience acknowledged. Recent neurological research has identified facial and pupillary biomarkers tied to tinnitus distress, offering a path toward objective recognition of patient suffering. Feeling heard is often the first step toward healing.
Useful Tip:
- Start with open-ended questions and empathetic listening.
- Acknowledge the emotional toll of tinnitus before offering next steps.
2) Clear, Evidence-Based Information
Patients are bombarded with conflicting online advice. They crave clear, clinically sound education. A 2024 European survey, spanning patients, clinicians, and researchers highlighted a shared interest in reliable information on tinnitus treatments, yet noticeable gaps in patient satisfaction with current care.
Clinician Insight:
- Offer structured educational materials on what treatments are supported by evidence and what outcomes are realistically achievable.
3) Patients Seek Effective, Accessible Therapies
Recent research underscores what works and what patients notice:
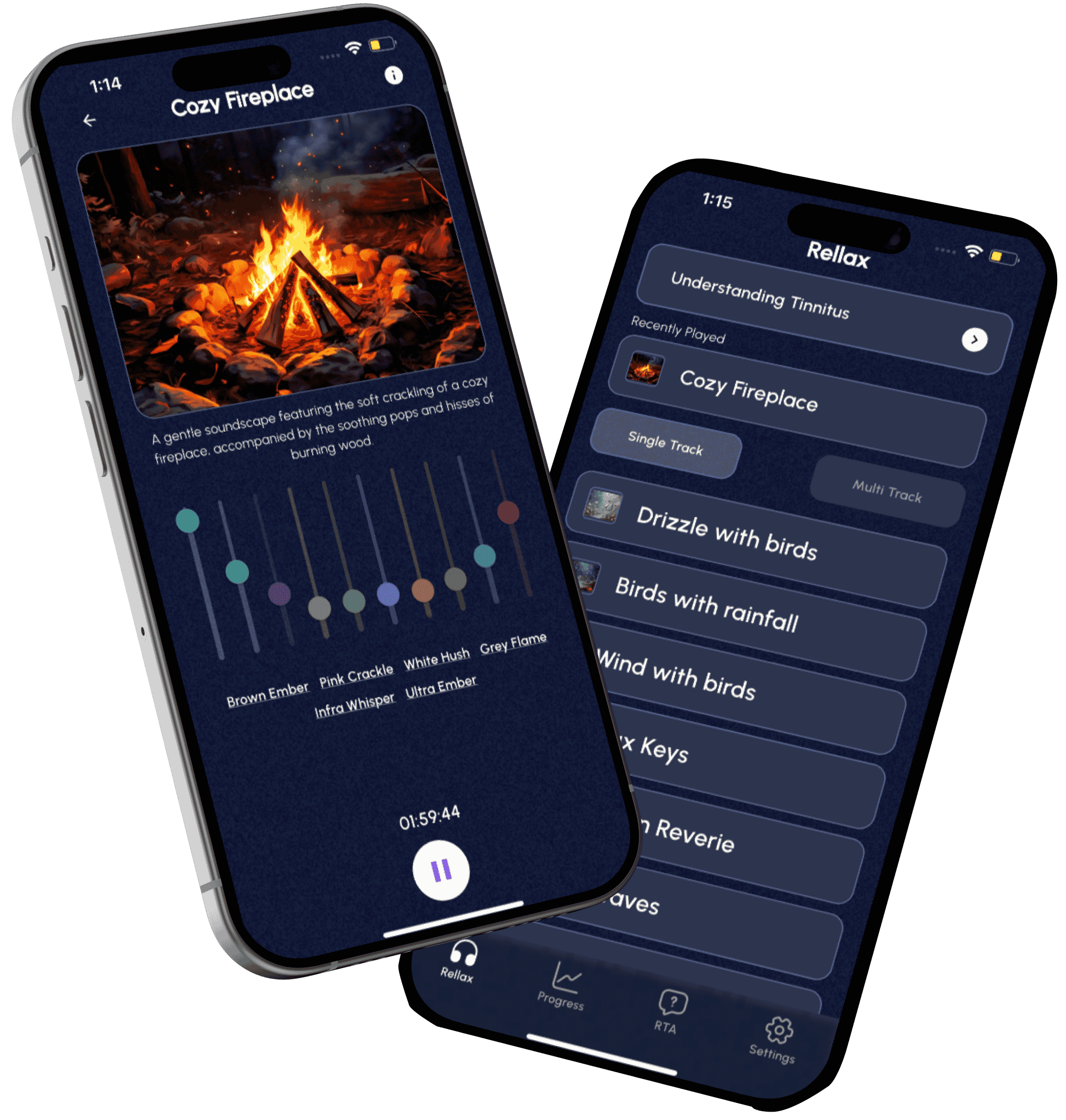
- App-based CBT and Sound Therapy: A pioneering app combining chatbot-guided CBT and sound therapy significantly reduced tinnitus distress in a small trial, comparable to in-person psychologist support.
- Hearing aids plus counseling: A 2025 report at ASHA’s World Tinnitus Week highlighted that combining amplification with informational counseling improved tinnitus outcomes, even in mild hearing loss cases.
- Neuromodulation & Biomarker-backed care: A breakthrough in objectively measuring tinnitus severity may soon allow therapies tailored to individual stress responses.
Clinic Application:
- Offer blended care: Combine in-clinic counseling with Rellax digital tools for TRT, CBT, sound therapy, and self-monitoring.
- Use objective metrics (when available) to track progress alongside patient-reported outcomes.
4) Mental Health Support
Tinnitus is often accompanied by anxiety, sleep issues, and impaired cognition. A 2025 study linked long-term tinnitus to deficits in attention and memory. Mental health support, especially CBT remains foundational for improving quality of life in tinnitus care.
Recommended Practice:
- Integrate structured mental health support into care plans.
- Provide Rellax-delivered TRT modules with clinician oversight.
5) Flexible, Personalized Care Models
One-size-fits-all doesn’t work. A 2024 review on clinical guidelines emphasized the need for individualized, stepwise diagnostic and treatment approaches across diverse healthcare contexts.
Implementation:
- Use a tiered care model: Assessment → education → in-clinic options + Rellax digital tools → follow-up.
- Customize interventions based on severity, patient preferences, and accessibility.
6) Hope and Measurable Progress
Chronic tinnitus often feels insurmountable. Yet, combining empathy, clear communication, and digital tools like Rellax can shift that perception. Offer milestones, track PROMs such as Tinnitus Handicap Inventory (THI), and celebrate improvements, even in distress or quality of life.

Summary Table: Aligning Care with Patient Priorities
| Patient Need | Action for Clinics |
| Validation & Recognition | Start consultations with empathetic listening; acknowledge distress. |
| Evidence-Based Guidance | Provide structured information and realistic outcome expectations. |
| Accessible Treatment Options | Offer Rellax TRT & sound therapy, hearing interventions, and blended pathways. |
| Mental Health Support | Integrate emotional coping strategies; Rellax modules can augment clinic care. |
| Personalized, Flexible Models | Use tiered, integrated plans with regular metrics. |
| Hope & Measurable Progress | Track and share patient milestones to foster control and optimism. |
Regional and Demographic Patterns That Affect Expectations
Patients’ expectations are influenced by culture, age, and health-system factors:
- Western systems often prioritize evidence-based therapies (TRT, structured counseling, and sound therapy).
- Some Asian contexts combine traditional medicine approaches with modern audiological care; communication about evidence and expectations is critical.
- Younger patients are more open to digital tinnitus therapy and apps, while older patients may prefer face-to-face reassurance and gradual rehabilitation.
How Technology is Shaping Patient-Centered Tinnitus Care
The last decade has seen a major shift in how patients expect to access healthcare and tinnitus management is no exception. While in-clinic care remains essential, technology is now playing a vital role in extending support beyond the consultation room.
24/7 Access to Relief Tools
Patients no longer want to wait for their next appointment to find relief. Mobile apps and sound therapy tools provide instant access to white noise, relaxation exercises, and mindfulness techniques whenever tinnitus feels overwhelming.
Data Tracking & Personalization
Digital platforms can track usage patterns, sleep quality, and self-reported distress. Over time, they adapt therapy to the individual, making treatment more personalized and responsive. For audiologists, this data creates a clearer picture of patient progress between visits.
Complementing In-Clinic Care
Technology doesn’t replace the clinic, it extends it. By integrating solutions like Rellax into treatment plans, clinicians can ensure patients have support between appointments, improving adherence, engagement, and long-term outcomes.

Where Clinics and Audiologists Commonly Miss the Mark
Insufficient explanation about prognosis and options
Patients leave confused about realistic outcomes.
Fragmented care pathways
Patients often move between GPs, ENT, and audiology without clear ownership of long-term management.
Lack of follow-up and self-management support
Patients want ongoing, accessible tools to manage flareups.
Practical fix:
Implement a structured tinnitus pathway (assessment → education + personalized plan → scheduled follow-up or digital program) and document shared decisions.
How to Translate Patient Insights into Clinical Practice (Practical Checklist)
- Start with listening: Make the first visit 60% patient story, 40% exam. Use validated questionnaires.
- Set realistic expectations: Explain evidence (e.g., CBT helps distress; sound therapy can reduce perception) and identify patient priorities (sleep, work, concentration).
- Offer a menu of options: Hearing optimization, CBT referral, sound therapy, lifestyle changes, and curated digital tools. Personalize the plan and schedule a follow-up within 4–8 weeks.
- Integrate digital tools thoughtfully: Prescribe apps that have clinical evidence or structured counseling, and pair them with clinician oversight.
- Measure outcomes: Track PROMs (THI, TFI) and patient satisfaction to refine care pathways.
Conclusion:
Above all, patients with tinnitus are looking for 3 things: relief, understanding, and practical help from credible sources. As audiologists and clinic leaders, aligning care to those priorities, through listening, clear education, personalized plans and evidence-informed digital tools improves outcomes and patient trust. Listening to patient voices (from surveys and qualitative studies) should shape both in-clinic practice and partnerships with digital platforms.
If your clinic is ready to offer patient-centered, measurable tinnitus care pathways that combine in-clinic assessment with evidence-based digital support, Rellax can help you integrate tools for sound therapy, structured counseling, and patient tracking into your patient flow. Contact Rellax for a demo and see how a blended care model improves engagement and outcomes.
Frequently Asked Questions (FAQs)
Have any question?
Do not hesitate to contact us. We’re a team of experts ready to talk to you.