Introduction
Did you know that over 50 million adults in the U.S. experience tinnitus at some point in their lives? For many, it’s more than a ringing, it can feel like a constant burden, intruding on sleep, focus, and emotional wellbeing. Imagine trying to relax after a long day, only to hear a sound no one else notices, a high-pitched buzz, a whoosh, or a persistent hum.
As a clinician, your role isn’t just to diagnose a symptom; it’s to educate patients about tinnitus and guide them through the treatments that can help. Education isn’t a lecture, it’s a conversation. It’s about giving patients the tools to understand their condition, engage with therapy, and feel empowered to take action.
In this article, we’ll share 5 actionable strategies to educate patients about tinnitus and their treatment options, helping them move from confusion to confidence and from feeling overwhelmed to feeling supported.

1. Start With the Story: Understanding Before Treating
Patients often arrive anxious, having read online forums or watched videos. They may worry and ask questions like“Will I go crazy from this sound?” or “Is this permanent?”
The first step is listening. Invite patients to describe:
- The sound itself
- When it started
- How it affects sleep, work, or daily life
Once you understand their story, focus on connecting what they’re feeling to why it’s happening. Help them make sense of their experience, how tinnitus relates to hearing changes, stress, or environmental triggers and what factors might be shaping how they perceive it.
When patients start to see the “why” behind their symptoms, the conversation shifts from frustration to understanding. That clarity builds trust and makes them more open to learning about the next steps you’ll recommend.
2. Clarify What Tinnitus Is (and Treatment Goals)
Many patients assume tinnitus is an “ear issue,” but it’s often linked to the brain’s auditory processing, stress, or circulation. Your role as a clinician is to clarify that tinnitus isn’t a disease, it’s a symptom of how the brain reacts to missing or altered sound input.
Help patients understand that the goal of treatment is to retrain the brain’s response, reduce distress, and improve quality of life, not to erase the sound altogether.
Encourage them to report sudden hearing changes immediately; early intervention can make a difference.
Use visuals or short animations to explain what’s happening in the auditory pathway and what “management” really means, so they see the science, not just hear it.
3. Connect Education to Action: Introduce Modern Treatment Tools
Once patients understand what tinnitus is, guide them to actionable treatment options. Evidence shows a multi-pronged approach is most effective:
- Sound and Auditory Rehabilitation: Hearing aids, sound generators, or digital sound therapy
- Cognitive Approaches: CBT or counseling to reframe perception of tinnitus
- Lifestyle and Environmental Adjustments: Daily habits to reduce intensity
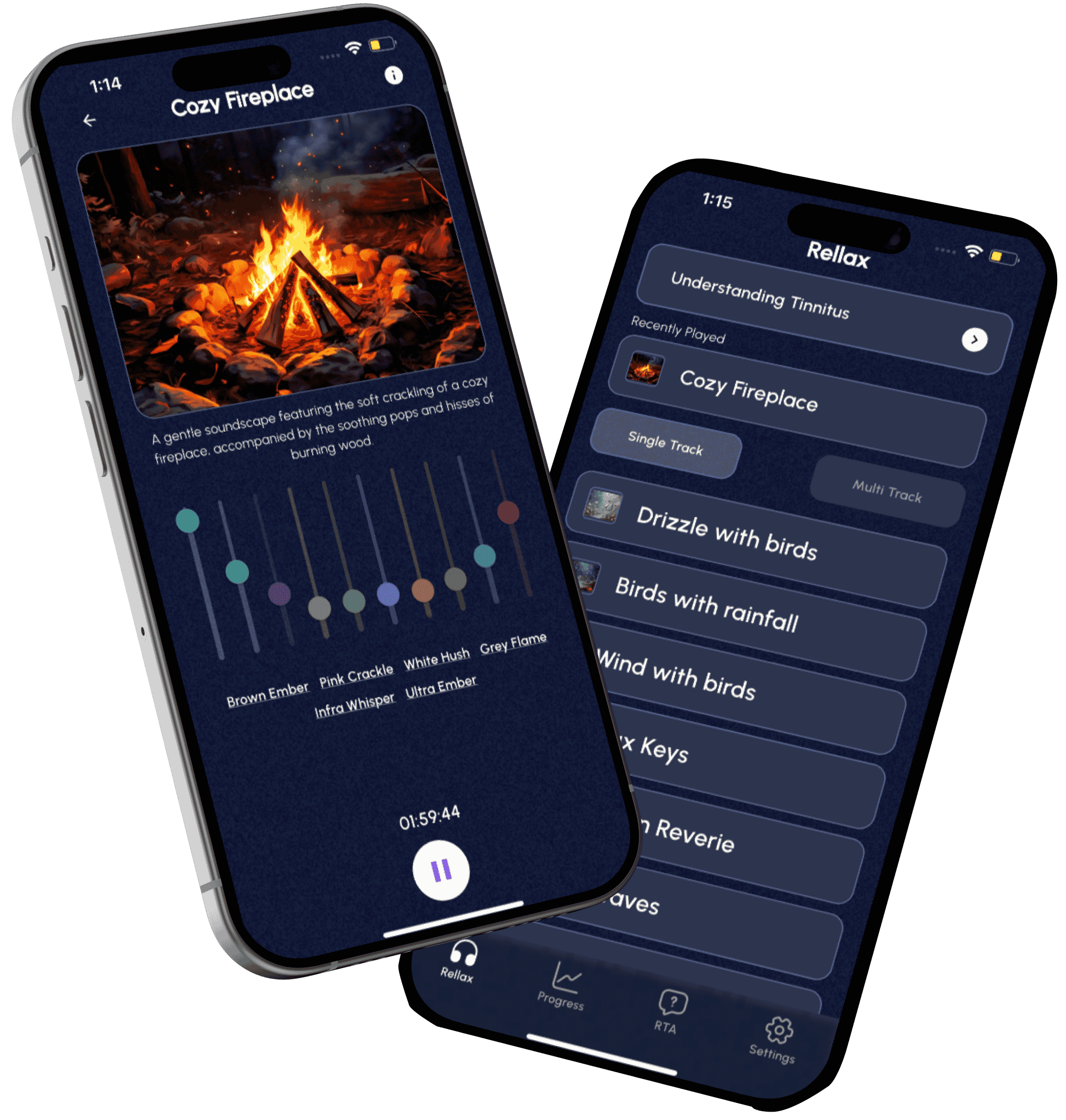
Clinician tip: Digital tools like Rellax can extend care beyond the clinic. Patients can access personalized sound therapy, track progress, and practice relaxation exercises. This supports treatment adherence and allows you to review outcomes during follow-ups.
4. Empower Lifestyle and Environmental Management
Treatment isn’t limited to devices or therapy sessions, daily life matters. Teach patients that small daily habits can make a big difference:
- Noise Management: Avoid prolonged loud exposure; use ear protection in high-decibel environments, but avoid total silence.
- Healthy Routines: Balanced diet, exercise, stable sleep schedule, and limiting caffeine/alcohol before bed.
- Stress Reduction: Yoga, deep breathing, mindfulness, and short meditation sessions. Evidence shows these reduce emotional burden.

Encourage patients to use a tinnitus journal to recognize daily patterns such as when symptoms spike or ease, so they can adjust habits more confidently.
Lifestyle Focus | Patient Action | Treatment Benefit |
Noise exposure | Ear protection in loud settings | Reduce symptom spikes |
Sleep | Consistent bedtime & wake-up | Improve rest and therapy effectiveness |
Stress | Mindfulness/relaxation | Reduce distress and perception of tinnitus |
Diet & exercise | Balanced nutrition & activity | Support neurological and auditory health |
Lifestyle guidance reinforces therapy and empowers patients to feel in control of their treatment journey.
5. Manage Expectations and Reinforce Hope
Patients may hear “there’s no cure” and feel discouraged. Your framing makes all the difference: “There’s no universal cure yet, but there are proven ways to manage tinnitus and improve your quality of life.”
Focus on gradual, functional improvements like better sleep, fewer spikes, improved concentration, and reduced emotional distress. Review progress together during follow-ups, and highlight even small wins to keep motivation high.
Conclusion:
Helping patients understand tinnitus isn’t just about sharing facts, it’s about building trust and guiding them toward hope. When clinicians listen first, explain clearly, and use modern tools and education, patients feel supported instead of overwhelmed. With empathy and evidence on your side, every conversation becomes a step toward relief and confidence.
For a modern, patient-centered companion to extend care beyond the clinic, consider Rellax, which combines therapy tracking, sound modules, and guided relaxation to support patients every step of the way.
“When education inspires action, even the quietest progress sounds like relief.”
Frequently Asked Questions (FAQs)
Ask about sound patterns, pulse synchronization, and onset history. Pulsatile tinnitus often requires vascular evaluation, unlike subjective tinnitus.
Currently, no universal FDA-approved cure exists. However, sound-based therapies, behavioral interventions, and digital tools have strong clinical evidence for symptom management.
Daily use of sound therapy, regular check-ins, and supportive tools like Rellax help maintain motivation and track progress.
Adequate rest, stress management, balanced diet, and avoiding prolonged noise exposure can significantly ease symptoms.
Use empathy, relatable analogies, progress tracking, and patient-friendly technology to bridge understanding and action.
Have any question?
Do not hesitate to contact us. We’re a team of experts ready to talk to you.